I have often shared my occupational therapy journey from beginning as an OTA and then becoming an OT. While at the same time going from feeling burned out and discouraged in my OT practice to a passion-filled practice which fills my OT cup! I feel that my OT journey is just getting started, and I love sharing my discoveries with other OTs, OTAs and students so they can avoid many of the pitfalls I have experienced in my career.
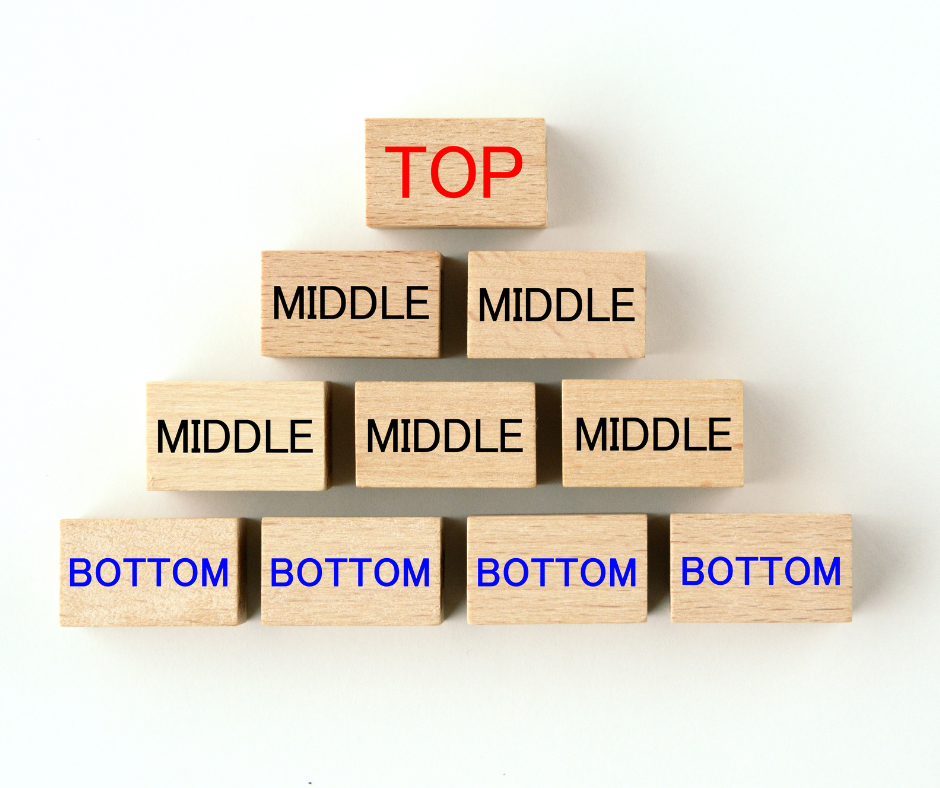
As I have been completing research for several courses that we are creating, I have come across literature discussing the top-down approach vs the bottom-up approach. This concept has had a significant influence on my practice in last 8 years, second only to occupation-based practice. I practiced for many years under a bottom-up approach, which focuses first on the deficits or impairments that could impact function or performance of an occupation, such as strength, range of motion, cognition, coordination, and sensory processing, which are believed to be prerequisites for occupational performance. The bottom-up approach assumes that restoring motor, cognitive and psychological skills will lead to successful performance in activities or occupations. (Weinstock-Zlotnick & Hinojosa, 2004).
In contrast, the top-down approach begins with assessing engagement in meaningful occupations within the client's contexts; this includes the meaning of the occupations and their relevance to the client's identity. The next step is to determine whether the client can participate in those meaningful occupations as well as the probable reasons for any identified occupational dysfunction. In a top-down approach, performance skills, performance patterns, context and client factors are considered later vs in the bottom-up approach they are considered first. (Weinstock-Zlotnick & Hinojosa, 2004). Some literature refers to bottom-up approaches as impairment-focused and top-down as task-specific therapeutic approaches. (Katelyn, et al, 2019).
Bottoms Up Approach Example
Evaluation of a client:
• OT assessment: upper extremity range of motion and manual muscle testing, balance, coordination, sensation, vision, cognition and ADL performance
• Findings: the client requires assistance with bathing and dressing , bilateral upper extremity strength of 4-/5 grossly, standing balance is fair, and impaired fine motor coordination per the Nine Hole Peg Test.
• Treatment Plan: improve upper extremity strength, standing balance and fine motor coordination with the long term goal for independence in bathing and dressing
Top Down Approach Example
Evaluation of a client:
• Client reports being concerns that she is unable to bath standing in her shower.
• OT assessment: performance skills, performance patterns, client factors and contexts reveals that client has showered with their spouse for the last 45 years, but is currently not able to engage in showering. It is determined the client's standing balance is fair and presents with edema in both feet which impairs her standing balance in the shower.
• OT continues to ask questions finds out the following from the client:
○ She has received therapy in the past for balance and she does not wish to participate in additional treatment for balance
○ A shower chair or bench is not an option because there will not be enough room for her spouse to shower at the same time
• Treatment plan: The goal will be that the client will be able to safely shower with the spouse from stand utilizing DME. The spouse will assist with actual bathing as this is a form of intimacy for the spouse and the client. The spouse will be trained in how to safely provide physical support if needed.
Top-down approaches seem to be the most compatible with client-centered approaches. Bottom-up approaches can also be used with client-centered approaches but pose a greater risk for the therapist setting goals instead of the client setting the goals. Evidence indicates that functional outcomes are best achieved utilizing a top-down, task-specific therapeutic approaches. Studies also indicate that impairment-based treatments are effective in improving the targeted impairment, but they do not necessarily transfer over to improved functional performance (Katelyn, et al, 2019).
I think for me I was most surprised by the findings that gains made toward targeted impairments did not necessarily mean that an individual would demonstrate improved ability to complete an actual task. When I first became aware of this information, my first thoughts were to wonder how I would do an evaluation without assessing things like strength and coordination. I have found that despite their impact on occupational performance, most payors and organizations expect these factors to be assessed. I have found that what works for me is to utilize a top down approach by developing an occupational profile , as I wrote about in my last blog, to determine what occupations are meaningful to the client and assess their ability to engage in those occupations. I then assess the performance patterns, performance skills, client factors and contexts such as strength, ROM, cognition, coordination, pain, coping strategies, balance, social supports, environment and psychosocial factors to determine which are impacting the identified occupational dysfunction. I review my findings with my client and we collaboratively develop the goals as well as the treatment plan. If impairments are identified that do not impact occupational performance or the client does not wish to address, I do not include those areas in my treatment plan.
The challenge for OTs, OTAs and students working in health care settings, is that most medical models utilize bottom-down approaches. Fortunately, we are seeing more evidence to support the use of biopsychosocial models to address health and wellness. Top-down approaches are more compatible within these models.
So what responses do I get from my clients since I have transitioned to using a top-down approach?
A majority are extremely positive. On a weekly basis I am told things like "I feel like you listened to me, I am so glad we are going to address these areas". "So you aren't going to have me do pegs? I am so glad, I still don't know why they had me do those in rehab". "Why hasn’t anyone addressed these things until now?". Using a top-down approach has helped to better guide my clinical reasoning and help me to feel confident that I am providing client-centered care. I know It would be easy to focus on just the positive comments. I wish that every single one of my clients who I recommended services to were agreeable to OT treatment, but I don't think that will ever be the case for any clinician of any discipline. I don't always have success with clients, but I have seen a significant decrease in the amount of clients who decline OT services after an evaluation. I no longer find myself trying to convince clients to participate in certain treatment interventions, because we are addressing the occupations that they want to address. I feel like my clients are more satisfied and I am definitely more gratified in my OT practice.
If you found this blog helpful, share it with others. If you have questions or comments for us, we want to hear them! Contact us at info@AspireOT.us